Foodborne Diseases Active Surveillance Network
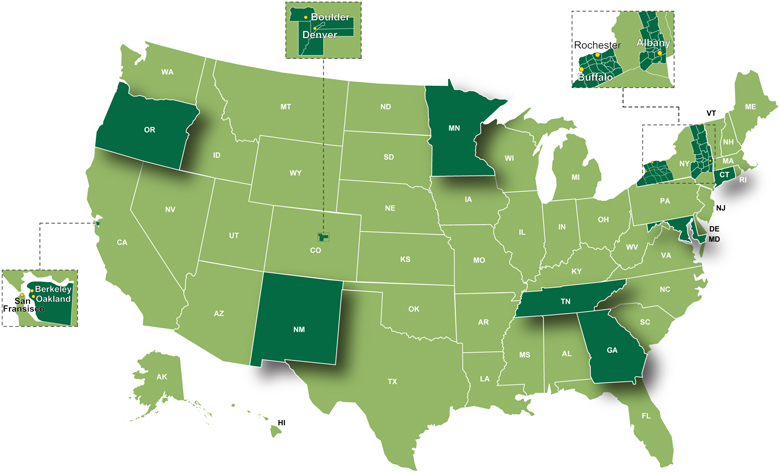
The Foodborne Diseases Active Surveillance Network (FoodNet) is the principal foodborne disease component of the Centers for Disease Control and Prevention (CDC) Emerging Infections Program (EIP). Nationwide, FoodNet is a collaborative program among the CDC, USDA, FDA, and ten US states. The New Mexico Emerging Infections Program (NMEIP) FoodNet program, a partnership between the NMDOH and the UNM, began active surveillance on January 1, 2004. Active, state-wide surveillance is conducted through audits at all microbiology laboratories in the state and several laboratories in Texas that serve New Mexico residents.
When the above pathogens are identified by laboratory testing in clinical specimens from residents of New Mexico, FoodNet personnel complete a case report form, collecting such information as basic demographics, hospitalizations, and potential exposures to the pathogens. Data from all ten of the FoodNet sites are aggregated by CDC to produce national estimates of disease.
The objectives of FoodNet are:
- Determine the burden of foodborne disease in the United States.
- Monitor trends in the burden of specific foodborne illnesses over time.
- Attribute the burden of foodborne illness to specific foods and settings.
- Develop and assess interventions to reduce the burden of foodborne illness.
FoodNet also participates in various special projects looking at antimicrobial resistance patterns of enteric pathogens by submitting selected bacterial isolates to the CDC, antimicrobial resistance patterns in retail meat products, risk factors for specific pathogens and Hemolytic Uremic Syndrome (HUS), and laboratory practices associated with the use of culture versus non-culture laboratory methods.
FoodNet Data
- Visit the FoodNet Trends, Data Tables & Figures page for national FoodNet data.
- Visit the New Mexico Infectious Disease Data page for New Mexico data on these pathogens.
Special Projects
National Antimicrobial Resistance Monitoring System (NARMS)
The National Antimicrobial Resistance Monitoring System (NARMS) was established in 1996, within the framework of the Centers for Disease Control and Prevention (CDC) Emerging Infections Programs (EIP) Foodborne Diseases Active Surveillance Network (FoodNet) and the CDC Epidemiology and Laboratory Capacity (ELC) for Infectious Diseases Program. NMEIP has been participating in NARMS since 2004. The primary objective of this project is to monitor antimicrobial resistance among non-typhoidal Salmonella, Salmonella serotype Typhi, Salmonella serotype Paratyphi, Escherichia coli O157, and Shigella isolated from humans. The proportion of isolates submitted to NARMS varies by pathogen.
NARMS Retail Meat Study (RMS)
The RMS is a surveillance program initiated in 2002 by NARMS. The primary objective is to monitor the prevalence of antimicrobial resistance among foodborne bacteria, specifically Salmonella, Campylobacter, Enterococcus, and Escherichia coli. The results generated by the NARMS retail meat program serve as a reference point for identifying and analyzing trends in antimicrobial resistance among these organisms.[1] NMEIP started participating in the RMS in 2004. Retail meat samples are purchased from a random sample of stores within a three county radius of Albuquerque. The meat samples are aliquoted and tested at the Environmental Microbiology section of the Biology Bureau at the New Mexico Department of Health (NMDOH) Scientific Laboratory Division (SLD). Bacterial isolates are shipped to CDC and the Food and Drug Administration (FDA). This real-time surveillance has benefited foodborne outbreak investigators in determining the source of several outbreaks as they were unfolding.[2]
Pulsed-Field Gel Electrophoresis (PFGE) Cluster Project
This project aims to characterize PFGE clusters that are being investigated as possible outbreaks at FoodNet sites. From 2009-2011, the project collected data on how bacterial clusters were identified, factors that encouraged cluster investigation, and time lines. Data are in the analysis phase at CDC.
Research Studies
FoodNet Non-O157 Shiga Toxin-Producing E. coli Study: Assessment of Risk Factors for Laboratory-Confirmed Infections and Characterization of Illnesses by Microbiological Characteristics.
The primary objective of this case-control study is to identify risk factors for sporadic non-O157 shiga toxin-producing E. coli (STEC) infections and to estimate the proportion of disease risk attributable to specific risk factors. The study will also look at laboratory characterization of non-O157 STEC isolates in combination with clinical information collected through the study questionnaire and through routine public health surveillance. All persons with a laboratory-confirmed non-O157 STEC infection are eligible. For each STEC case enrolled, three controls will be recruited from the same county. A control is someone who did not get sick with an STEC infection. New Mexico initiated study enrollment in July 2012 and will continue through July 2015.
Escherichia coli O157:H7 Infection: Antibiotic Exposure and the Risk of Hemolytic Uremic Syndrome (HUS)
The primary objective of the study was to provide an estimate of the association between antibiotic exposure and HUS among persons infected with E. coli O157. Other risk factors and predictors of HUS will also be evaluated including the microbiologic characteristics of infecting E. coli O157 strains and host factors. This study was conducted at all 10 FoodNet sites. In New Mexico, persons with a laboratory- confirmed E. coli O157 infection between May 2006 and June 2010 were eligible. Participation included informed verbal consent, a phone interview with the patient and chart review, when applicable. De-identified data generated by this project from each participating EIP site was submitted to CDC for analysis.
Genetic Predictors of Developing Hemolytic Uremic Syndrome (HUS) Following Infection With Shiga Toxin-Producing Escherichia coli (STEC)
The primary objective of this study is to identify human genomic factors associated with the development of HUS among persons infected with STEC and calculate the proportion of disease risk attributable to these genetic factors. The identification of such genetic factors will contribute to a better understanding of the pathogenesis of the disease and potentially have therapeutic and preventive implications, by providing a mechanism for identifying persons at highest risk of HUS for preventive education or tailoring of therapy based on immunologic risk factors.
Participants in the E. coli O157 cohort study (above) were asked to participate in the genomics study. When the cohort study ended, the genomic study period was extended and the inclusion criteria modified to include all persons diagnosed with an STEC infection. Participation included informed written consent and a saliva specimen sent to a CDC/FoodNet affiliate laboratory. Enrollment has ended and analysis is currently underway at CDC.
References
- Retail Meat Report 2010
National Antimicrobial Resistance Monitoring System. Accessed December 4, 2012. - Ensuring a Safer Food Supply: Surveillance of New Mexico’s Retail Meat
Butler L, Lathrop S, Torres P. New Mexico Epidemiology, Volume 2012,Number 5, June 29, 2012.

